nul n est prophete dsurtout et exclusivement dans les pays sous developpes qui font fuir pas uniquement les harraguas mais leurs meilleurs cadres ? et on ose parler de recherche ?????

What is chlamydia?
Chlamydia is a common sexually transmitted disease (STD) caused by a bacterium. Chlamydia can infect both men and women and can cause serious, permanent damage to a woman's reproductive organs.
How common is chlamydia?
Chlamydia is the most frequently reported bacterial sexually transmitted infection in the United States. In 2011, 1,412,791 cases of chlamydia were reported to CDC from 50 states and the District of Columbia, but an estimated 2.86 million infections occur annually. A large number of cases are not reported because most people with chlamydia do not have symptoms and do not seek testing. Chlamydia is most common among young people. It is estimated that 1 in 15 sexually active females aged 14-19 years has chlamydia.
How do people get chlamydia?
People get chlamydia by having sex with someone who has the infection. “Having sex” means anal, vaginal, or oral sex. Chlamydia can still be transmitted even if a man does not ejaculate. People who have had chlamydia and have been treated can get infected again if they have sex with an infected person.
Chlamydia can also be spread from an infected woman to her baby during childbirth.
Who is at risk for chlamydia?
Any sexually active person can be infected with chlamydia. It is a very common STD, especially among young people. It is estimated that 1 in 15 sexually active females aged 14-19 years has chlamydia.
Sexually active young people are at high risk of acquiring chlamydia for a combination of behavioral and biological reasons. Men who have sex with men (MSM) are also at risk for chlamydial infection since chlamydia can be transmitted by oral or anal sex.
What are the symptoms of chlamydia?
Chlamydia is known as a ‘silent’ infection because most infected people have no symptoms. If symptoms do occur, they may not appear until several weeks after exposure. Even when it causes no symptoms, chlamydia can damage a woman’s reproductive organs.
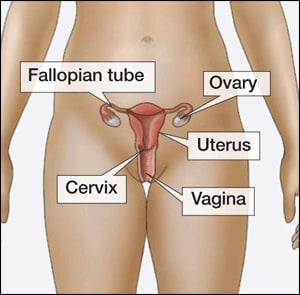
In women, the bacteria first infect the cervix (structure that connects the vagina or birth canal to the uterus or womb) and/or the urethra (urine canal). Some infected women have an abnormal vaginal discharge or a burning sensation when urinating. Untreated infections can spread upward to the uterus and fallopian tubes (tubes that carry fertilized eggs from the ovaries to the uterus), causing pelvic inflammatory disease (PID). PID can be silent, or can cause symptoms such as abdominal and pelvic pain. Even if PID causes no symptoms initially, it can lead to infertility (not being able to get pregnant) and other complications later on.
Some infected men have discharge from their penis or a burning sensation when urinating. Pain and swelling in one or both testicles (known as “epididymitis”) may also occur, but is less common.
Chlamydia can also infect the rectum in men and women, either through receptive anal sex, or possibly via spread from the cervix and vagina. While these infections often cause no symptoms, they can cause rectal pain, discharge, and/or bleeding (known as “proctitis”).
What complications can result from chlamydial infection?
The initial damage that chlamydia causes often goes unnoticed. However, chlamydial infections can lead to serious health problems.
In women, untreated infection can spread upward to the uterus and fallopian tubes (tubes that carry fertilized eggs from the ovaries to the uterus), causing pelvic inflammatory disease (PID). PID can be silent, or can cause symptoms such as abdominal and pelvic pain. Both symptomatic and silent PID can cause permanent damage to a woman’s reproductive tract and lead to long-term pelvic pain, inability to get pregnant, and potentially deadly ectopic pregnancy (pregnancy outside the uterus).
In pregnant women, untreated chlamydia has been associated with pre-term delivery, and can spread to the newborn, causing an eye infection or pneumonia.
Complications are rare in men. Infection sometimes spreads to the tube that carries sperm from the testis, causing pain, fever, and, rarely, preventing a man from being able to father children.
What about chlamydia and HIV?
Untreated chlamydia may increase a person’s chances of acquiring or transmitting HIV – the virus that causes AIDS.
How does chlamydia affect a pregnant woman and her baby?
In pregnant women, untreated chlamydia has been associated with pre-term delivery, and can spread to the newborn, causing an eye infection or pneumonia. Screening and treatment of chlamydia during pregnancy is the best way to prevent these complications. All pregnant women should be screened for chlamydia at their first prenatal visit.
Who should be tested for chlamydia?
Any sexually active person can be infected with chlamydia. Anyone with genital symptoms such as discharge, burning during urination, unusual sores, or rash should avoid having sex until they are able to see a health care provider about their symptoms.
Also, anyone with an oral, anal, or vaginal sex partner who has been recently diagnosed with an STD should see a health care provider for evaluation.

Find an STD testing site near you.
CDC recommends yearly chlamydia testing for all sexually active women age 25 or younger and older women with risk factors for chlamydial infections (e.g., women who have a new or more than one sex partner), and all pregnant women. Any woman who is sexually active should discuss her risk factors with a health care provider who can then determine if more frequent testing is necessary.
Men who have sex with men (MSM) who have receptive anal sex should be tested for chlamydia each year. MSM who have multiple and/or anonymous sex partners should be tested more frequently.
HIV-infected sexually active women who are age 25 or younger or have other risk factors, and all HIV-infected patients who report having receptive anal sex should be tested for chlamydia at their first HIV care visit and then at least annually. A patient’s health care provider might determine more frequent testing is necessary, based on the patient’s risk factors.
How is chlamydia diagnosed?
There are laboratory tests to diagnose chlamydia. Specimens commonly used for testing include a cotton swab of the vagina (collected by the woman herself or her health care provider) or a urine sample.
What is the treatment for chlamydia?
Chlamydia can be easily treated and cured with antibiotics. HIV-positive persons with chlamydia should receive the same treatment as those who are HIV-negative.
Persons with chlamydia should abstain from having sex for seven days after single dose antibiotics, or until completion of a seven-day course of antibiotics, to prevent spreading the infection to partners.
Repeat infection with chlamydia is common. Persons whose sex partners have not been appropriately treated are at high risk for re-infection. Having multiple chlamydial infections increases a woman's risk of serious reproductive health complications, including pelvic inflammatory disease and ectopic pregnancy. Women and men with chlamydia should be retested about three months after treatment of an initial infection, regardless of whether they believe that their sex partners were successfully treated.
Infants infected with chlamydia may develop conjunctivitis (infection of the membrane lining the eyelids) and/or pneumonia. Chlamydial infection in infants can be treated with antibiotics.
What about partners?
If a person has been diagnosed and treated for chlamydia, he or she should tell all anal, vaginal, or oral sex partners from the past 2 months so that they can see a healthcare provider and be treated. This will reduce the risk that the sex partners will develop serious complications from chlamydia and will also reduce the person’s risk of becoming re-infected. A person with chlamydia and all of his or her sex partners must avoid having sex until they have completed their treatment for chlamydia (i.e., seven days after a single dose of antibiotics or until completion of a seven-day course of antibiotics) and until they no longer have symptoms. For tips on talking to partners about sex and STD testing, visit www.gytnow.org/talking-to-your-partner/![]()
To help get partners treated quickly, healthcare providers may give patients extra medicine or prescriptions to give to their sex partners. This is called expedited partner therapy or EPT. EPT is only available in some parts of the country. Consult a healthcare provider to find out if it is available in a specific area. Sex partners should still be encouraged to see a healthcare provider, regardless of whether they receive EPT.
How can chlamydia be prevented?
Latex male condoms, when used consistently and correctly, can reduce the risk of getting or giving chlamydia. The surest way to avoid chlamydia is to abstain from vaginal, anal, and oral sex or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
What can be expected from the cytologic examination of cervicovaginal smears for the diagnosis of Chlamydia trachomatis infections?
Source
Laboratories of Histology, Faculty of Medicine, Louis Pasteur University, Strasbourg, France.
Abstract
The value of Papanicolaou-stained smears for the diagnosis of chlamydial infections is still disputed. A comparative examination of smears from infected and uninfected women has allowed the proposal of a new scheme for the interpretation of the cytologic abnormalities associated with chlamydial infection. In particular, the appearances of metaplastic cells were classified, and two smear types were found to have the highest sensitivities and positive predictive values: smears in which the metaplastic cells had (1) intracytoplasmic vacuoles containing polymorphonuclear leukocytes or (2) numerous small intracytoplasmic vacuoles containing a central eosinophilic granule. The sensitivity of this method is low, however; cytology cannot replace bacteriologic identification for the diagnosis of chlamydial infections. Nevertheless, the examination of Papanicolaou-stained smears could be considered as a screening tool in low-risk populations; provided that all of the cytologic features were considered, presumptive diagnoses of chlamydial infections could be obtained.
Alerte aux Chlamydiae !
Alors qu'elles sont actuellement relativement rares, certaines bactéries telles que le gonocoque ou le tréponème pâle sont encore associées à des noms de maladies très évocatrices - "chaude-pisse" ou "vérole" - bien ancrés dans le vocabulaire populaire. Ceci est d'autant plus surprenant, qu'à l'inverse, le germe qui est actuellement responsable de la majorité des maladies sexuellement transmissibles d'origine bactérienne est désigné exclusivement par son nom scientifique : Chlamydia trachomatis. Ceci paraît injustifié puisqu'au moins 5 % des femmes (jusqu'à 20 % pour certaines études) et 3 à 7 % des hommes hébergent ce germe responsable d'une grande partie des infertilités.
La présence fréquente de "Chlamydia trachomatis" (CT), en particulier chez les jeunes, est expliquée par son caractère très contagieux (le germe est transmis lors de rapports sexuels non protégés) ainsi que par son "côté sournois". Cette bactérie est en effet fréquemment hébergée par des hommes et des femmes qui ne présentent aucun signe de maladie. Ces "porteurs sains" peuvent cependant développer une véritable infection.
 Alors qu'elles peuvent intéresser les yeux, le péritoine et les articulations, les infections à "C. trachomatis" touchent essentiellement l'appareil urogénital. Le germe se développe dans les cellules de la muqueuse de l'urètre ainsi qu'au niveau du col de l'utérus chez les femmes. Il peut alors ne donner aucune manifestation d'infection, mais rester très contagieux, ou entraîner une maladie plus ou moins bruyante.
Alors qu'elles peuvent intéresser les yeux, le péritoine et les articulations, les infections à "C. trachomatis" touchent essentiellement l'appareil urogénital. Le germe se développe dans les cellules de la muqueuse de l'urètre ainsi qu'au niveau du col de l'utérus chez les femmes. Il peut alors ne donner aucune manifestation d'infection, mais rester très contagieux, ou entraîner une maladie plus ou moins bruyante.
Sournoise Chlamydia
Chez l'homme, l'infection à "Chlamydia trachomatis" peut ainsi se manifester par une urétrite se traduisant par des brûlures lorsque l'on urine, des écoulements ou de simples picotements passant presque inaperçus. Une infection de l'épididyme (épididymite) ou de la prostate (prostatite) peut y être associée.
Chez la femme, "C. trachomatis" est fréquemment asymptomatique, mais peut également se traduire par des signes évoquant une infection urinaire ou une mycose. Surtout, le germe peut entraîner des infections génitales hautes avec atteinte de l'utérus et des trompes : endométrites et salpingites, qui peuvent se présenter sur un mode aigu, très bruyant avec fièvre et douleurs pelviennes. Le diagnostic est alors rarement méconnu. Mais le risque de ces infections génitales hautes est d'évoluer fréquemment de façon plus chronique avec peu de signes (pas de fièvre, peu ou pas de douleurs) et d'être non ou mal traitées. La fertilité de ces femmes est directement menacée avec un risque de stérilité tubaire de 20 % et un risque de grossesse extra-utérine de 10 %.
- PMID:
- 3201874
- [PubMed - indexed for MEDLINE]https://www.blog4ever.com/gestion/articles/composer
-
www.laboratoriosilesia.com/upfiles/sibi/GI030743.pdfthese cases.2 Krieger et al.,3 however, reported a specificity and ... smear microscopy, Wiese et al.4 concluded that as .... Genital tract infection with Chlamydia trachomatis is common .... Sekhri A, Le Faou AE, Tardieu JC, Antz M, Fabre M.www.ncbi.nlm.nih.gov/pmc/articles/PMC1194684/Pooled specimens for Chlamydia trachomatis: new approach to increase yield and cost .... [PubMed]; Sekhri A, Le Faou AE, Tardieu JC, Antz M, Fabre M. What can be .... Eschenbach DA, Paavonen J, Lingenfelter J, Bell T, Zabriskie V, et al.europepmc.org/articles/PMC1194684/pdf/genitmed00039-007...Certain serovars of Chlamydia trachomatis, as the ..... by Kaneti et al,"7 diagnosing a current infection in an ..... 31 Sekhri A, Le Faou AE, Tardieu JC, Antz M,.bu.umc.edu.dz/theses/biologie/SAY5458.pdfJ'adresse mes plus sincères remerciements à Monsieur SEKHRI ..... soit par une infection bactérienne (chlamydia trachomatis, Gardnerella vaginalis). ‹ soit par
Sekhri, A (A)
Latest papers:
Division of Cardiology, Department of Medicine, New York Medical College, Valhalla, NY 10595, USA. ROBERT_LERNER@nymc.eduBACKGROUND Warfarin affects the synthesis and function of the matrix Gla-protein, a vitamin K-dependent protein, which is a potent inhibitor of tissue calcification. OBJECTIVES To investigate the incidence of mitral valve calcium (MVC), mitral annular calcium (MAC) and aortic valve calcium (AVC) in patients with non-valvular atrial fibrillation (AF) treated with warfarin vs. no warfarin. PATIENTS AND METHODS Of 1155 patients, mean age 74 years, with AF, 725 (63%) were treated with warfarin and 430 (37%) without warfarin. The incidence of MVC, MAC and AVC was investigated in these 1155 patients with two-dimensional echocardiograms. Unadjusted logistic regression analysis was conducted to examine the association between the use of warfarin and the incidence of MVC, MAC or AVC. Logistic regression analyses were also conducted to investigate whether the relationship stands after adjustment for confounding risk factors such as age, sex, race, ejection fraction, smoking, hypertension, diabetes, dyslipidemia, coronary artery disease (CAD), glomerular filtration rate, calcium, phosphorus, calcium-phosphorus product, alkaline phosphatase, use of aspirin, beta blockers, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and statins. RESULTS There was a significant association between the use of warfarin and the risk of calcification [unadjusted odds ratio = 1.71, 95% CI =(1.34-2.18)]. The association still stands after adjustment for confounding risk factors. MVC, MAC or AVC was present in 473 of 725 patients (65%) on warfarin vs. 225 of 430 patients (52%) not on warfarin (P < 0.0001). Whether this is a causal relationship remains unknown. CONCLUSIONS Use of warfarin in patients with AF is associated with an increased prevalence of MVC, MAC or AVC.Acta Cytol. ;32 (6):805-10 3201874 Cit:6Laboratories of Histology, Faculty of Medicine, Louis Pasteur University, Strasbourg, France.The value of Papanicolaou-stained smears for the diagnosis of chlamydial infections is still disputed. A comparative examination of smears from infected and uninfected women has allowed the proposal of a new scheme for the interpretation of the cytologic abnormalities associated with chlamydial infection. In particular, the appearances of metaplastic cells were classified, and two smear types were found to have the highest sensitivities and positive predictive values: smears in which the metaplastic cells had (1) intracytoplasmic vacuoles containing polymorphonuclear leukocytes or (2) numerous small intracytoplasmic vacuoles containing a central eosinophilic granule. The sensitivity of this method is low, however; cytology cannot replace bacteriologic identification for the diagnosis of chlamydial infections. Nevertheless, the examination of Papanicolaou-stained smears could be considered as a screening tool in low-risk populations; provided that all of the cytologic features were considered, presumptive diagnoses of chlamydial infections could be obtained.Most cited papers:
Acta Cytol. ;32 (6):805-10 3201874 Cit:6Laboratories of Histology, Faculty of Medicine, Louis Pasteur University, Strasbourg, France.The value of Papanicolaou-stained smears for the diagnosis of chlamydial infections is still disputed. A comparative examination of smears from infected and uninfected women has allowed the proposal of a new scheme for the interpretation of the cytologic abnormalities associated with chlamydial infection. In particular, the appearances of metaplastic cells were classified, and two smear types were found to have the highest sensitivities and positive predictive values: smears in which the metaplastic cells had (1) intracytoplasmic vacuoles containing polymorphonuclear leukocytes or (2) numerous small intracytoplasmic vacuoles containing a central eosinophilic granule. The sensitivity of this method is low, however; cytology cannot replace bacteriologic identification for the diagnosis of chlamydial infections. Nevertheless, the examination of Papanicolaou-stained smears could be considered as a screening tool in low-risk populations; provided that all of the cytologic features were considered, presumptive diagnoses of chlamydial infections could be obtained.Division of Cardiology, Department of Medicine, New York Medical College, Valhalla, NY 10595, USA. ROBERT_LERNER@nymc.eduBACKGROUND Warfarin affects the synthesis and function of the matrix Gla-protein, a vitamin K-dependent protein, which is a potent inhibitor of tissue calcification. OBJECTIVES To investigate the incidence of mitral valve calcium (MVC), mitral annular calcium (MAC) and aortic valve calcium (AVC) in patients with non-valvular atrial fibrillation (AF) treated with warfarin vs. no warfarin. PATIENTS AND METHODS Of 1155 patients, mean age 74 years, with AF, 725 (63%) were treated with warfarin and 430 (37%) without warfarin. The incidence of MVC, MAC and AVC was investigated in these 1155 patients with two-dimensional echocardiograms. Unadjusted logistic regression analysis was conducted to examine the association between the use of warfarin and the incidence of MVC, MAC or AVC. Logistic regression analyses were also conducted to investigate whether the relationship stands after adjustment for confounding risk factors such as age, sex, race, ejection fraction, smoking, hypertension, diabetes, dyslipidemia, coronary artery disease (CAD), glomerular filtration rate, calcium, phosphorus, calcium-phosphorus product, alkaline phosphatase, use of aspirin, beta blockers, angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, and statins. RESULTS There was a significant association between the use of warfarin and the risk of calcification [unadjusted odds ratio = 1.71, 95% CI =(1.34-2.18)]. The association still stands after adjustment for confounding risk factors. MVC, MAC or AVC was present in 473 of 725 patients (65%) on warfarin vs. 225 of 430 patients (52%) not on warfarin (P < 0.0001). Whether this is a causal relationship remains unknown. CONCLUSIONS Use of warfarin in patients with AF is associated with an increased prevalence of MVC, MAC
Inscrivez-vous au blog
Soyez prévenu par email des prochaines mises à jour
Rejoignez les 9 autres membres








